Inicio / Super Cialis
"Purchase super cialis cheap online, erectile dysfunction treatment in tampa".
By: W. Jose, M.A., Ph.D.
Assistant Professor, Chicago Medical School of Rosalind Franklin University of Medicine and Science
Certain cognitive disorders erectile dysfunction natural remedies over the counter herbs buy super cialis 80mg lowest price, such as dementia or delirium erectile dysfunction mayo effective 80mg super cialis, may also qualify as mental disease or defect erectile dysfunction protocol ingredients order on line super cialis, depending on circumstances and jurisdiction erectile dysfunction doctor austin order genuine super cialis line. Forensic psychiatrists take different approaches in relating clinical diagnoses to an insanity standard. Most experts believe that a psychiatric diagnosis should be made whenever possible. Case law or statutes may specify jurisdictional definitions of mental disease or defect. In the absence of specific definitions, trends in case law and standards for the admissibility of expert testimony may provide guidance. Acceptable practices for the establishment of mental disease or defect should contain at least a narrative description of a scientifically based disorder, symptom cluster, or syndrome. Generally speaking, the use of specific diagnoses helps the expert organize patterns of symptoms and explain the conclusions drawn. Establishing the Relationship Between Mental Disease or Defect and Criminal Behavior Once the presence or absence of a mental disease or defect is established, the psychiatrist focuses on the relationship, if any, between the mental disease or defect and the alleged crime. Although such a history may be relevant, the psychiatrist should state the limitations of rendering an insanity opinion based solely on that history. Understanding what motivates a person to behave criminally is important when studying the relationship between mental illness and criminal acts. Analyzing the criminal intent of defendants involves examining their awareness of what they were doing during the crime and what their motivations for actions taken were at that time. In particular, the psychiatrist inquires as to how the defendant felt before, during, and after the criminal acts. Finally, the psychiatrist should carefully consider the possibility that defendants may, to avoid criminal prosecution, fabricate or exaggerate psychiatric symptoms and past psychiatric illness. They may misrepresent their motivations or intent regarding their criminal behavior, as well as any emotions they experienced while committing the crime. Conducting collateral interviews, reviewing collateral records, and administering appropriate psychological testing can assist clarification of possible malingering. Since each case is unique, the importance, weight, and combination of each of the three areas of analysis will vary. That is why relying on just one factor may be inappropriate in certain situations. The forensic psychiatrist should strive for a consistent approach to the analysis to ensure a thorough review of all data and reliable testimony. Relationship Between Mental Disease or Disorder, Criminal Behavior, and the Legal Standard In formulating the opinion, the psychiatrist considers to what degree the mental condition and its relationship to the alleged crime meet the legal standard for criminal responsibility. When an individual is charged with multiple offenses, the psychiatrist generally conducts the insanity analysis for each offense. Because the legal standards for determining insanity vary between states and the federal system, an individual could theoretically be found insane in one jurisdiction and sane in another. Regardless of the test used, psychiatrists should explain how they determined that the defendant did or did not meet the legal standard for insanity. Some states have substituted appreciate, understand, recognize, distinguish, or differentiate for know. Some state courts have interpreted the word appreciate to represent a broader reasoning ability than know. The type of wrongfulness can be determined by statute or case law or can be left to the discretion of the jury. The interpretation, however, is specific to the jurisdiction, although the general intent is to broaden the standard. An example of the variations in interpreting know and appreciate is the contrasting testimony of Dr. In that trial, the applicable standard was whether the defendant lacked the substantial capacity to appreciate the wrongfulness of his conduct. The prosecution argued that the correct interpretation of appreciate was the consideration of cognitive function, excluding affective impairment or moral acknowledgment. The defense argued that appreciation went beyond the mere cognitive acknowledgment that the act was wrong and encompassed the "affective and emotional understanding of his conduct" (Ref. Carpenter testified: So that I do think that he had a purely intellectual appreciation that it was illegal. Emotionally he could give no weight to that because other factors weighed far heavier in his emotional appreciation.
These sleep spindles occur simultaneously on both sides and what causes erectile dysfunction in diabetes purchase super cialis australia, although maximal centrally erectile dysfunction vacuum pump super cialis 80mg line, are widespread xarelto impotence order super cialis australia. They are monophasic and generally of no more than 50 V in amplitude; although they are seen bilaterally erectile dysfunction 20s cheap super cialis 80mg overnight delivery, they are not synchronous. Furthermore, they are not rhythmic and can be seen at irregular intervals of anywhere from several to one per second. When the general amplitude is reduced to below 20 V, it is helpful to be able to compare the current record with past ones, or to make serial recordings in order to determine whether the low amplitude is stable or worsening. It is also critical to ensure that the recording is made during relaxed wakefulness: tense or anxious patients, or those engaging in some more or less demanding mental activity, will have low-amplitude recordings. A generalized decrease in amplitude may be seen in conditions characterized by widespread cortical neuronal loss. In evaluating amplitude asymmetries of the alpha rhythm, one must not forget that the left side normally has an amplitude of up to 50 percent less than the right; it is thus only when the alpha rhythm on the left is at least 50 percent less than that on the right that one can declare with certainty that an abnormality is present. The beta rhythm is generally bilaterally symmetric, but even here an amplitude asymmetry is not unusual in normal individuals; thus, for the beta rhythm, any asymmetry must be more than 35 percent before it can be declared outside the normal range. A unilateral reduction in amplitude of the beta rhythm indicates a frontal lesion. In general, a unilateral reduction of the alpha rhythm suggests a lesion of the underlying occipital cortex, but in the case of the alpha rhythm an amplitude reduction may also be seen with distant lesions in the frontal or parietal cortices or the ipsilateral thalamus. Here, in conditions where the skull has been breached, for example with a burr hole or fracture (regardless of how much scar tissue has formed), an excessive amplitude is seen on the side with the breach, making the normal amplitude activity on the other side appear low by comparison (Cobb et al. Focal slowing Focal slowing may consist of either theta or delta activity, and is seen in a variety of focal conditions, including infarcts and tumors (Daly and Thomas 1958; Gastaut et al. Generalized slowing Generalized slowing appears in the theta or delta range and may be either bilaterally asynchronous or synchronous. Asynchronous generalized slowing is most commonly seen in metabolic or toxic delirium (Pro and Wells 1977; Romano and Engel 1944). Metabolic deliria accompanied by generalized asynchronous slowing include hepatic encephalopathy and uremic encephalopathy, and the deliria occurring secondary to hyperglycemia, hypoglycemia, hypernatremia, hyponatremia, hypercalcemia, or hypocalcemia. Toxic deliria associated with similar slowing include those due to phenytoin (Roseman 1961), valproate (Adams et al. Interestingly, however, the delirium of delirium tremens, rather than slowing, is accompanied by an increase of beta activity (Kennard et al. The delirium seen with bacterial meningitis or viral encephalitis is also marked by generalized slowing. A mild degree of generalized asynchronous slowing may also be seen as a normal variant in a small minority of subjects; furthermore, occasional scattered theta transients are not at all abnormal in normal subjects over the age of 60 years (Kooi et al. Generalized slowing also, of course, occurs with sleep, and thus slowing in a drowsy patient who is slipping in and out of sleep is of little significance. Interictal activity Interictal activity consists of what are known as epileptiform discharges. These paroxysmal transients may consist of isolated spikes or sharp waves or may appear as complexes, such as spike-and-sharp wave, spike-and-slow wave, sharp-and-slow wave, polyspikes, or polyspike-and-wave discharges. Although epileptiform activity may be seen in a very small percentage of subjects who have never had a seizure (Ajmone-Marsan and Zivin 1970; Gibbs et al. Focal epileptiform activity strongly suggests an underlying focal epileptogenic lesion. The task of localizing focal epileptiform activity is facilitated by having in mind a spatial image of the electrical activity itself. With this image in mind, one can understand the changes produced on either a referential or bipolar montage. Thus, proceeding from Fp1 to F3 the depth falls, from F3 to C3 it continues to fall to its nadir, from C3 to P3 it rises, and from P3 to O1 it continues to rise back to the surface. Furthermore, assume also that electrode F3, being over the gently downsloping wall of the chasm, sees a potential of 50 V, and that electrode C3, being over the nadir of the chasm, sees a potential of 100 V. Electrode P3, being over the following wall of the chasm, sees 50 V, and electrode O1 encompasses the normal landscape of 25 V. As noted earlier, in a referential recording each scalp, or active electrode, is paired with the same reference electrode, in this example the ipsilateral ear; thus, in this example, as Fp1 F7 F3 Fz Cz Fp2 F8 F4 A1 T3 C3 100 V C4 T4 A2 P3 T5 50 V Pz P4 T6 O1 25 V O2 Figure 1. Thus, with referential recordings, it is the channel showing the greatest amplitude that serves to localize the focus of the electrical paroxysm. The situation with bipolar recordings is quite different: here, it is not amplitude that is important but a phenomenon known as phase reversal (Knott 1985; Lesser 1985).
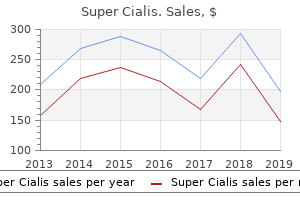
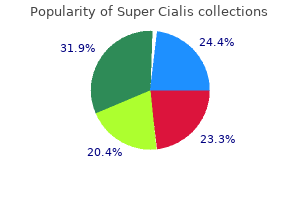
Buy cheapest super cialis and super cialis. What Is The Best Erectile Dysfunction Drug?.
Cited in "Leading Drugs for Psychosis Come Under New Scrutiny" Erica Goode erectile dysfunction 2015 purchase super cialis online now, the New York Times erectile dysfunction drugs history order 80mg super cialis with mastercard, May 20 erectile dysfunction drug approved to treat bph symptoms effective super cialis 80 mg, 2003 "Brain Volume Changes After Withdrawal of Atypical Antipsychotics in Patients with First-episode Schizophrenia" G xylometazoline erectile dysfunction buy super cialis 80mg. Apr;31(2):146-53 2011 "The Case Against Antipsychotic Drugs: a 50 Year Record of Doing More Harm Than Good" Robert Whitaker, Med Hypotheses. Cohen, Psychotherapy and Psychosomatics 74:145-153, 2005 the Myth of the Chemical Cure Joanna Moncrieff, Palgrave Macmillan, 2008. Analysis of a State Hospital Inpatient Population" "The Latest Mania: Selling Bipolar Disorder" David "Long-term Antipsychotic Treatment and Brain Volumes" Beng-Choon Ho, et al. Whitfield, the International Journal of Risk & Safety in Medicine 22 (2010) "Psychiatric Drug Promotion and the Politics of Neoliberalism" by Joanna Moncrieff "Soteria and Other Alternatives to Acute Psychiatric Hospitalization: A Personal and Professional Review" Loren Mosher Journal of Nervous and Mental Disease. Rappaport, International Pharmacopsychiatry 13, 100-11, 1978 "Prejudice and Schizophrenia: a Review of the "Mental Illness is an Illness Like Any Other" Approach" Read, John el al. The intent of this document is to support the development of an Open Dialogue practice for whole teams participating in Open Dialogue meetings, for supervision and training purposes, and for helping in systematic research. Starting in 1984, at Keropudas Hospital in Tornio, Finland, staff already trained in family therapy decided to change the way inpatient admissions were handled. Following the work of Yrjц Alanen (1997), they altered their response to acute crises by having a network meeting, bringing together the person in distress, their family, other natural supports, and any professionals involved, in advance of any decision about hospitalization. This was the birth of a new, open practice that evolved-in tandem with continued clinical innovation, organizational change, and research-into what has come to be known as "Open Dialogue, " first described as such in 1995 (Aaltonen Seikkula, & Lehtinen, 2011; Seikkula et al. The "openness" of Open Dialogue refers to the transparency of the therapy planning and decision-making processes, which take place while everyone is present. Over a ten-year period, this formerly traditional inpatient facility in Tornio was transformed into a comprehensive psychiatric system with continuity of care across community, outpatient, and inpatient settings. The practice of Open Dialogue thus has two fundamental features: (1), a community-based, integrated treatment system that engages families and social networks from the very beginning of their seeking help; and (2), a "Dialogic Practice, " or distinct form of therapeutic conversation within the "treatment meeting. The treatment meeting constitutes the key therapeutic context of Open Dialogue by unifying the professionals and the network into a collaborative enterprise. Thus, Dialogic Practice is embedded in a larger psychiatric service that shares its premises, because it is essential to have both aspects. The Open Dialogue approach is an integrative one in which other therapeutic modalities (Ziedonis, Fulwiler, Tonelli, 2014; Ziedonis et al, 2005; Ziedonis 2004) can be added, adapted to the needs of the person and family, as part of an unfolding and flexible "treatment web" (Hald, 2013; Seikkula & Arnkil 2014). For the purposes of this discussion on Dialogic Practice, the two principles of "dialogue (polyphony)" and "tolerance of uncertainty" will be given special attention as the foundation of therapeutic conversation within the treatment meeting. The other five of the seven principles, which emphasize the organizational features of the system, will be explicated in another document on organizational change and the system fidelity characteristics (Ziedonis, Seikkula, & Olson, in preparation). This companion document on organizational change will describe different ways that the Open Dialogue principles and the treatment meeting have been integrated into clinical practice, treatment programs, agencies, and systems of care. The following discussion will focus on the twelve, key elements of fidelity to Dialogic Practice that characterize the therapeutic, interactive style of Open Dialogue in face-to-face encounters within the treatment meeting. Open Dialogue involves being able to listen and adapt to the particular context and language of every exchange. For this reason, it is not possible here to make specific recommendations for sessions in advance, or for invariant phases in the treatment process. Prescribing this form of detailed structure could actually work against the process of Open Dialogue. It is the unique interaction among the unique group of participants engaging in an inevitably idiosyncratic therapeutic conversation that provides the possibilities for positive change. While every dialogue is unique, there are distinct elements, or conversational actions on the part of the therapists, that generate and promote the flow of dialogue and, in turn, help mobilize the resources of the person at the center of concern and the network. Dialogic Practice is based on a special kind of interaction, in which the basic feature is that each participant feels heard and responded to . With an emphasis on listening and responding, Open Dialogue fosters the co-existence of multiple, separate, and equally valid "voices, " or points of view, within the treatment meeting. Within a "polyphonic conversation, " there is space for each voice, thus reducing the gap between the so-called "sick" and "well. Evaluating the dialogical quality of a conversation means, first and foremost, evaluating the responsiveness of the therapists. Among the first steps is often for one of the therapists to engage with the person at the center of the crisis in a careful, detailed, back-and-forth interchange. As illustrated below, having input from the network assists in shedding further light on the nature of the crisis. The dialogical therapist invites each person in the meeting to share their perspective and the various, related issues that come up during the conversation.
Associative visual agnosia may occur secondary to bilateral infarction of the medial occipitotemporal cortex and subcortical white matter cialis causes erectile dysfunction purchase super cialis 80mg visa, especially involving the lingual erectile dysfunction treatment centers purchase 80 mg super cialis mastercard, fusiform erectile dysfunction ayurvedic drugs cheap 80mg super cialis with mastercard, and parahippocampal gyri (Albert et al erectile dysfunction natural buy super cialis once a day. Cases have also been reported secondary to a left unilateral occipitotemporal infarct coupled with infarction of the splenium of the corpus callosum (Feinberg et al. Theoretically, it appears reasonable to say that in the apperceptive subtype the destruction of the secondary p 02. In the associative subtype, sparing of the secondary visual cortices allows for the development of an image, but destruction of the more anterior occipitotemporal cortex renders impossible an association between the image and the concepts that the patient has regarding various objects. The anomic patient, upon handling the pair of scissors, will still remain unable to come up with the name, whereas the agnosic patient will recognize and name the object. Anomic aphasia may also appear similar to tactile agnosia in that anomic patients also are unable to name an object by touching it. In contrast with tactile agnosia, however, patients with anomic aphasia are unable to name the object although they can describe its use. Auditory agnosia Auditory agnosia, or, more explicitly, environmental auditory agnosia, is a very rare condition characterized by an inability to recognize such environmental sounds as the ringing of a telephone or the honking of a horn, despite normal hearing and a normal ability to understand the spoken word (Vignolo 1982). Tactile agnosia Tactile agnosia is characterized by an inability to recognize objects by touching and handling them, despite normal light touch, pin-prick, vibratory and two-point discriminatory sensation, and despite an ability to describe the shape of the object in question (Platz 1996). If the patient has any difficulty in doing so, ask for a description of the object. At this point, ask the patient to take a look at the object and name it: in tactile agnosia, the patient will be able to name it immediately by sight. Importantly, because tactile agnosia may occur unilaterally in either hand it is necessary to test both hands, using a different object each time; furthermore, it is also necessary to tell the patient to use only one hand at a time and not to palpate the object with both hands. Auditory agnosia may come to attention when patients fail to answer the phone or perhaps, with potentially disastrous consequences, fail to respond to the honking of a car horn. Bedside testing may be accomplished by standing behind the patient and ringing a bell or perhaps snapping your fingers, and then asking the patient what he heard. In environmental auditory agnosia, patients will acknowledge hearing something but they will be unable to say what it was. In all these cases, the prosopagnosia occurred as part of a stroke syndrome, generally secondary to ischemic infarction. Prosopagnosia has also been noted secondary to resection of the posterior portion of the right temporal lobe (Mesad et al. There are also rare reports of progressive prosopagnosia occurring secondary to progressive atrophy of the right temporal lobe (Evans et al. Finally, there are also rare reports of prosopagnosia occurring on a developmental basis (Kress and Daum 2003). Remarkably, these patients, although unable to identify others by their facial features, may be able to identify them by other features, such as their voice, dress, or characteristic gait (Damasio et al. Finally, and most remarkably, some patients are not able to recognize themselves when they look in the mirror (Damasio et al. As might be expected, such patients, in addition to being unable to recognize old acquaintances by their facial features, are also unable to utilize facial features to recognize new acquaintances (Malone et al. Topographagnosia At the outset, it should be noted that there is some debate regarding the definition of topographagnosia and, consequently, the reader, in perusing journal articles, should pay particular attention to the definition peculiar to the authors of the article. In this text, topographagnosia refers to a condition in which patients, despite adequate memory and vision, are unable to find their way in surroundings that had not previously caused any difficulty. In landmark agnosia, difficulty arises at the level of recognizing the Bank as a landmark. Although the patient may recognize the building, and even describe it, it is not recognized as a landmark and hence the patient is as likely to walk past it as to turn. In one case, a patient `had sudden difficulty finding her way out of a subway station she had used daily for years. The buildings in front of him were familiar to him, so he could recognize them right away. The basis for this, however, lies in an inability to commit to memory features of the new environment, and this stands in contrast with topographagnosia wherein memory is intact. Furthermore, patients with amnesia typically have no trouble finding their way in environments that they have travelled in before, provided, of course, that any retrograde amnesia has not obscured their recall.
Si quieres mantenerte informado de todos nuestros servicios, puedes comunicarte con nosotros y recibirás información actualizada a tu correo electrónico.

Cualquier uso de este sitio constituye su acuerdo con los términos y condiciones y política de privacidad para los que hay enlaces abajo.
Copyright 2019 • E.S.E Hospital Regional Norte • Todos los Derechos Reservados
